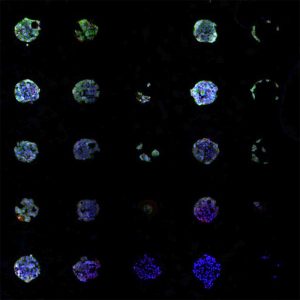
A chemical array screens for malignant melanoma cell types. Each dot contains a different combination of protein segments derived from the tumor environment. Credit: Kristopher Kilian
Malignant melanoma in dogs.
Just as in people, malignant melanoma is a type of skin cancer in dogs that affects pigmented cells known as melanocytes. Dogs often develop benign tumors in pigmented cells that do not metastasize, which are called melanocytomas. These tumors are found on areas of the dog’s body that have hair.
Most malignant melanomas occur on the mouth or mucous membranes, although about 10% of the time they are found on parts of the body covered with hair. They tend to grow extremely fast and are likely to spread to other organs, including the lungs and liver.
No one knows exactly why melanomas develop, although genetic factors seem to play a role. Additionally, trauma or compulsive licking of a particular spot on the skin may increase the likelihood that cells will multiply, thereby raising the chances that cells will mutate during the division process and become cancerous.
The research reported on human melanoma treatment in the article below may some day prove beneficial in the treatment of malignant melanoma in dogs as well.
May 26, 2017 by Liz Ahlberg Touchstone
From: Medical Press
Melanoma is a particularly difficult cancer to treat once it has metastasized, spreading throughout the body. University of Illinois researchers are using chemistry to find the deadly, elusive malignant cells within a melanoma tumor that hold the potential to spread.
Once found, the stemlike metastatic cells can be cultured and screened for their response to a variety of anti-cancer drugs, providing the patient with an individualized treatment plan based on their own cells.
“The vast majority of suffering in cancer is caused by metastasis, and these stemlike cells are believed to be the culprit,” said Kristopher Kilian, a professor of bioengineering and of materials science and engineering who led the research. “But when you take a patient’s cells from a biopsy or excised tumor, they lose their stem cell characteristics once you take them out of the body. We are using chemistry to make designer surfaces to reprogram them to that stemlike state.”
Kilian’s team focused on proteins found in the tumor’s environment within the body. They took 12 protein segments that bind to the surface of cancer cells, then mixed and matched them into 78 different combinations in an effort to recreate the body’s complex chemical environment.
The researchers created arrays of chemical combinations on glass slides and cultured mouse melanoma cells on them to see which combinations triggered the cells to return to their metastatic state. They published their findings in the journal ACS Central Science.
“A plastic dish coated with these simple peptide combinations could be used to take a patient’s cells, reactivate them to a stemlike state, and screen drugs on them. It’s a way to efficiently generate these stemlike metastatic cells to develop patient-specific models for individualized medicine,” Kilian said.
Screening drugs to specifically target the stemlike cells is important because they may not respond to the same drug that targets the main tumor, Kilian said.
The researchers said the array technique for finding stemlike cancer cells could work for many different types of cancer. They currently are working on breast and prostate cancers.
“This is where having a high-throughput technique like an array is very powerful,” Kilian said. “If you have all the chemical combinations on a single chip, you find out which ones work. If you can isolate the metastatic cancer cells, you can understand them, and then you can treat them.”








