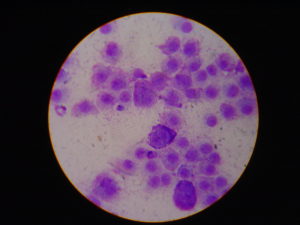
Microscopic appearance of mast cells.
More on Mast Cell Tumors in Dogs – A Common Canine Skin Cancer
A few blog posts ago, we posted a piece on mast cell tumors by Dr. Sue Ettinger, DVM, Dip. ACVIM (Oncology). We thought this would be a great follow-up article, as it’s a little more detailed. The more educated we become about these cancers, the more able we are to identify them early, and possibly treat them effectively.
The article below is from Critical Care DVM.
March 20, 2017
Mast cells are unique cells of the immune system that are involved in the body’s response to inflammation and allergies. Unfortunately, these cells can become cancerous to affect different areas of the body, particularly the skin. Given their commonality in our canine companions, I wanted to dedicate some time to sharing information about them. Please consider sharing this post with other dog parents. Happy reading!
Mast Cell Tumors – What are they?
Mast cells come from the bone marrow and ultimately end up in connective tissue throughout the body, particularly the skin. Each mast cell contains important granules composed of various chemicals like histamine, heparin, serotonin, and special enzymes that break down proteins. These chemicals play protective roles in wound healing, promote new blood vessel formation (called angiogenesis), and help the body defend against certain infectious organisms.
To date, we don’t truly know what causes mast cell tumors to form. Some studies have suggested fragile chromosomes that are unstable and prone to damage. Alterations in certain proteins (i.e.: p21 & p27), enzymes (i.e.: cyclin dependent kinase), and receptors (i.e.: kit) may play a role in the development of mast cell tumors. Approximately 20-30% of all mast cell tumors have a mutation in the gene for the kit receptor – the gene is called c-Kit. Occasionally, chronic inflammation and certain skin irritants have been implicated in tumor development as well.
Mast Cell Tumors – What do they look like?
Mast cell tumors are the most common skin tumors in dogs, accounting ~20% of all skin-associated tumors. These tumors are typically solitary masses in or underneath the skin. These lumps have quite a variable appearance. They may appear haired and minimally elevated to ulcerated and swollen. For this reason, pet parents should remember no one – not even a veterinarian – can simply look at or touch a skin mass and know what it is. Testing, like a fine needle aspiration or biopsy, must be done. As DrSueCancerVet says, #WhyWaitAspirate!
Older dogs are over-represented for developing mast cell tumors. There is no known gender predilection. Some breeds are affected more than others:
· Boxers
· Labrador Retrievers
· Beagles
· Schnauzers
· Boston Terriers
· Pugs
· Bulldogs
· Shar Peis
· Staffordshire Terriers
· Golden Retrievers
· Weimeraners
· Rhodesian Ridgebacks
When mast cells release their granules into the bloodstream – a process called degranulation – local and systemic complications are possible, including:
· Reddening and bleeding around the wound
· Fluctuation in the size of the tumor
· Stomach ulceration
· Low blood pressure
· Shock
As I mentioned earlier, mast cell tumors are most commonly found in or under the skin. Relative to that location, approximately 25% are found on the limbs and most are found on the trunk. Some locations are associated with a worse prognosis:
· On the prepuce of male dogs
· Peri-anal region
· Oral cavity
· Nail bed
· Mucocutaneous junctions
Mast Cell Tumors – How are they diagnosed?
Parents should have any skin mass larger than a pea or that has been present for more than one month evaluated by a veterinarian. This evaluation should include a minimally invasive procedure called a fine needle aspiration. In brief, a vaccine-sized needle is inserted into a skin mass and some cells are aspirated from it. The cells are examined under the microscope. Mast cells are readily identifiable, but confirmation with a board-certified veterinary clinical pathologist is recommended.
Once a mast cell tumor has been confirmed, additional testing is recommended. First and foremost, the mass should be completely removed via surgery. This is called an excisional biopsy. Depending on the location on the body, this task may be easy or exceedingly complicated. Partnering with a board-certified veterinary surgeon may be very helpful for complicated masses.
Traditionally, mast cell tumors are graded on a three-tier system called the Patnaik system to classify their degree of proliferation:
· Grade I – least aggressive; least likely to spread to other organs
· Grade II – moderately locally aggressive; tend not to metastasize but can do so (unpredictable behavior)
· Grade III – highly locally aggressive; high likelihood of metastasis
More recently, a two-tiered system called the Kiupel system based on various microscopic characteristics has been promoted:
· High grade
· Low grade
As part of a biopsy evaluation, the tumor should be tested for possible genetic mutations. Specifically, screening for the c-Kit mutation may help guide therapy and provide prognostically useful information.
Veterinarians will recommend tests to figure out how involved the rest of the body is with the cancer. This testing is called clinical staging, and is done to learn if the mast cell tumor has metastasized or spread to other organs. Recommended staging diagnostic tests are:
· Blood & urine tests (i.e.: complete blood count, serum biochemical profile, urinalysis)
· Abdominal sonography
· Lymph node cytology
· Spleen & liver cytology
· Bone marrow sampling
· Chest radiographs (x-rays)
The stages of mast cell disease are detailed below:
· Stage 1: one tumor in the skin (dermis) | no lymph node involvement
· Stage 2: one tumor in skin | spread to regional lymph node noted
· Stage 3: multiple skin tumors or one infiltrating tumor | with or without regional lymph node involvement
· Stage 4: any tumor with distant metastasis | recurrence with metastasis
Patients with no clinical signs of illness related to a mast cell tumor are said to be in substage A, while those with clinical signs are classified in substage B.
Mast Cell Tumors – How are they treated?
The biopsy of a mast cell tumor provides information a veterinarian uses to determine whether additional therapy is indicated. Factors taken into consideration include:
· Tumor grade
· Completeness of surgical margins
· Clinical staging
Complete surgical excision is the treatment of choice for mast cell tumors. This intervention may be curative in dogs with grade I completely excised tumors. A veterinarian may recommend a second surgery if a tumor was not completely removed. Unfortunately, some body locations (i.e.: limb, head, etc.) preclude complete excision. For these patients, radiation therapy is recommended to achieve local control. Radiation therapy is a very effective treatment modality. Two-year control rates of 85-90% are expected for low- and intermediate-grade mast cell tumors are treated with radiation therapy.
Chemotherapy is beneficial for patients with high grade tumors, tumors that have metastasized, and/or incompletely removed mass. A common initial protocol is a combination of a corticosteroid (i.e.: prednisone) and an injectable medication called vinblastine. Dogs receive eight total doses of vinblastine. The first four doses are administered weekly, and ideally the dose is escalated/increased with each treatment until the maximum dose is reached at the fourth dose. The latter four treatments are given every other week. A tapering dose of a corticosteroid is prescribed, and this drug is discontinued when vinblastine treatment is complete. Vinblastine can cause gastrointestinal upset, bone marrow suppression, and injury to the skin at the injection site if the drug leaks out of the vein. The overall response rate to this therapy is ~50%, and the median duration of response is ~5 months (range: 1 to >22 months).
Additional treatment may be recommended after vinblastine and corticosteroid therapy. Veterinarians may prescribe a drug called toceranib|Palladia™ if a dog’s tumor has a mutation in a gene called C-kit. This gene codes for a specific receptor called kit. Kit belongs to a class of receptors called receptor tyrosine kinases (RTK). In mast cells, RTKs tightly control cell growth and proliferation. In some mast cell tumors, RTK mutations cause unregulated cell growth. Palladia™ is a receptor tyrosine kinase inhibitor (RTKI) approved by the United States Food and Drug Administration to treat canine mast cell tumors because it blocks the kit receptor. Potential side effects of Palladia™ include gastrointestinal upset, bone marrow suppression, lameness, muscle cramping, and excess protein in the urine. Patients receiving Palladia™ should not be concurrently treated with non-steroidal anti-inflammatory medications (NSAIDs).
Other chemotherapeutic drugs that may be used to treat mast cell tumors are CCNU|Lomustine™, vincristine, hydroxyurea, cyclophosphamide, chlorambucil, and masitinib|Kinavet™. Dog parents are strongly encouraged to consult with a board-certified veterinary oncologist to determine the most appropriate treatment(s) for their canine companion.
Dogs with mast cell tumors may benefit from other supportive medications to combat the effects of the chemicals within the granules inside mast cells. These drugs include:
· Antihistamines: diphenhydramine|Benadryl™, famotidine|Pepcid AC™, ranitidine|Zantac™, cimetidine|Tagamet™
· Antacids: omeprazole|Prilosec OTC™, sucralfate|Carafate™
The take-away message about mast cell tumors in dogs…
Mast cell tumors are the most common skin cancers in dogs. There is a marked degree of variation in the appearance and biologic behavior of these tumors. Approximately 65-80% remain local and don’t spread. Initial treatment includes surgery, and following interventions like radiation therapy and/or chemotherapy may also be recommended.
To find a board-certified veterinary oncologist, please visit the American College of Veterinary Internal Medicine.
To find a board-certified veterinary surgeon, please visit the American College of Veterinary Surgeons.








